INTRODUCTION
Since
the description of a case of gastritis with veno-capillary ectasia as a source of massive haemorrhage by
Rider et al in 19531 many cases have now been recognised. In 1984
Jabari et al2 further defined this condition as ‘watermelon stomach’
based on its endoscopic appearance. This condition appears to be a somewhat
rare entity. This is report of two cases of this disease, both encountered at
Hairmyres Hospital, Glasgow over a period of five years during which 2500
endoscopies were done.
CASE 1
A
64 years old lady was admitted for an episode of melena, which had been
preceded by one month of upper abdominal pain, against a long background of
dyspepsia. On examination she was found to be anaemic.
Investigations showed iron defici-ency anaemia
and haemoglobin (Hb) 10.5 g/dl. Stools were positive for occult blood. Barium
meal and follow through showed persistent narrowing and reduced distensibiltity
in region of gastric antrum. The muscosal pattern however appeared intact.
Upper G.I. endoscopy showed very striking red streaked appearance of antrum
with multiple small raised red lesions. Biospy from the lesion showed small
collection of telangiectatatic capillaries lined by prominent endothelial cells
and one vessel contained thrombus. Biospy from gastric area showed mild to
moderate active chronic gastritis. While she was under observation her stools
continued to be positive for occult blood. Her Hb fell to 9.2g/dl. She was
transfused. Repeat endoscopy showed essentially similar features. She was
subjected to Antrectomy and Billroth I anastomosis. Gross biopsy specimen of
pyloric antrum showed prominence of rugae with red streaks over the tips of
gastric folds. Small pectial foci were seen in mucosa. There were small groups
of blood vessels in submucosa. Histology showed several small groups of
superficially located dilated capillaries, some of which contained fibrin thrombus.
There was focal fibro-muscular proliferation in the lamina propria. The
submucosa was oedmatous. There were groups of ectatic venous channels. Her
haemoglobin remained stable at around 14g/dl after surgery during two years
follow up.
CASE2
A
73 years old woman was admitted for weight loss, malaise, dyspnoea and ankle
swelling. On examination she was anaemic. She also had atrial fibrillation and
signs of early congestive cardiac failure.
Her investigation showed iron deficiency anaemia due
to chronic blood loss and Hb 7.1g/dl. Stools were positive for occult blood.
ESR was high. Immunoglobulins showed very high IgM 8.47g/l (91%mean normal
adult value). Liver Function Tests showed mild elevation of ALT (45.2). Barium
meal and enema were normal.
She was treated for congestive cardiac failure. She
was transfused. As her symptoms remained unchanged with persistently low Hb, an
upper GI endoscopy was done to exclude primary gastric lesion.
The
gastric antrum was grossly abnormal with typical appearance of watermelon
stomach (Figure1).
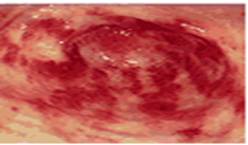 Figure 1: An upper endoscopy reveals
longitudinal erythematous stripes resembling stripes of a water melon
Figure 1: An upper endoscopy reveals
longitudinal erythematous stripes resembling stripes of a water melon
Biopsy
from the lesion showed small group of telangatatic vessels some of which
contained thrombus in lamina propria. In addition fibromuscular element was
present in mucosa.
She was advised surgery, which
she refused. She is still being followed up and remains rather tired and her
last checked Hb was 9.4g/dl
DISCUSSION
In
an elderly patient, especially in females persistent iron deficiency anaemia
with hypochlorydria or achlorhydria should warrant the diagnostic possibility
of gastric vascular ectasia. The mean age of presentation is 69.1 years (range
42-89 yrs). Patient most commonly present with chronic occult blood loss or
recurrent acute haemorrhage.3,4 The common clinical presentations
are iron deficiency anaemia (88%), Faecal Occult Blood (FOB) positive (42%),
Melena (15%), hematemesis (3%) and rarely hematochezia (1%).5 The
occult bleeding is transfusion dependent with a mean of 10 units over a
12-month period.
The aetiology of this condition remains unknown; one
theory being that water melon stomach is caused by recurrent episodes of antral
mucosal prolapse into pylorus that leads to mucosal trauma and ischemia.
Other conditions are associated with this condition.
In one series3 the most common associated disorders were Raynaud’s
phenomenon (31%) and sclerodactely (18%). Other associated conditions include
hypothyroidism, primary biliary cirrhosis, diabetes mellitus and autoimmune
liver disease.3-7
The diagnostic endoscopic findings are both uniform
and remarkably characteristic, these include longitudinal rugal folds
transforming the antrum and converging on pylorus, each containing a visible
convoluted column of vessels, the aggregate resembling the stripes of water
melon.2
Other features
include gastritis with evidence of mucosal prolapse. Conventional radiology is
often non-specific. Both gross appearance of resected antrum and microscopic
picture is characteristic. The resected specimen shows thickened mucosa with
torturous submucosal venous channels. Microscopic picture may show dilatation
of muscoal capillaries with focal thrombosis and fibromuscular hyperplasia of lamina
propria1,2,
The therapeutic options are numerous for this
condition and need to be individualised. Improvement of anaemia with out
further iron supplementation following surgery in patients including one of our
own case (Case1) suggest that the most appropriate treatment for this condition
is antrectomy with Billroth I anastomosis, but their is mortality of 7.4%8
associated with this operation.
Endoscopic therapy has been shown to be effective
with a minimal mortality. Endoscopic therapy, including the NDYAG laser, argon
laser, heater probe, bipolar therapy have been effective as a treatment. The
number of endoscopic sessions needed varied between 3-4 sessions over period of
4-12 months.3,6,7,9-11
Pharmacological agents like prednisone,2,12
prednisolone,13,14 estrogen-progesterone preparations13
have been used with various success rates. Octreotide was not shown to be
effective.15
In conclusion, Watermelon stomach is an increasingly
recognisable cause of persistent acute or occult gastrointestinal bleeding,
especially in elderly women. Usually presenting as severe iron deficiency
anaemia and occult or overt gastrointestinal blood loss. Diagnosis is
endoscopic, with characteristic appearance of watermelon like linear stripes in
antrum. Histology is rarely needed to confirm the diagnosis. The important
thing is to recognise the characteristic lesion and carry out appropriate
endoscopic procedure, leading to healing of the lesion with significant
improvement in the anaemia and a reduction in the need for blood transfusions.
REFERENCE
1.
Rider
JA, Koltz AP, Kirsner JB. Gastritis with veno-capillary ectasia as source of
massive gastric hemorrhage. Gastroenterology 1953:24;118-23.
2.
Jabbari
M, Cherry R, Lough JO, Daly DS, Kinnear DG, Goresky CA. Gastric antral vascular
ectasia: the watermelon stomach. Gastroenterology 1984; 87:1165-70.
3.
Gostout
CJ, Viggiano TR, Ahlquist DA, Wang KK, Larson MV, Balm R. The clinical and
endoscopic spectrum of the watermelon stomach. J Clinical Gastroenterol 1992;
15:256-63.
4.
Merrett
MN, Machet D, Ring J, Desmond PV, Martin CJ. Watermelon stomach: an unusual
cause of chronic gastrointestinal blood loss. Aust N Z J Surg 1991;61:393-96.
5.
Gretz
JE, Achem SR. The watermelon stomach: clinical presentation, diagnosis, and
treatment. Am J Gastroenterol 1998; 93:890-5.
6.
Gostout
CJ, Ahlquist DA, Radford CM, Viggiano TR, Bowyer BA, Balm RK. Endoscopic laser
therapy for watermelon stomach. Gastroenterology 1989;96:1462-5.
7.
Tsai
HH, Smith J, Danesh BJ. Successful control of bleeding from gastric antral
vascular ectasia (watermelon stomach) by laser photocoagulation. Gut 1991;
32:93-4.
8.
Borsch
G. Diffuse gastric antral vascular ectasia: the "watermelon stomach"
revisited. Am J Gastroenterol 1987; 82:1333-4.
9.
Bjorkman
DJ, Buchi KN. Endoscopic laser therapy of the watermelon stomach. Lasers Surg
Med 1992; 12:478-81.
10. Frager JD, Brandt LJ, Frank MS, Morecki
R. Treatment of a patient with watermelon stomach using transendoscopic laser
photocoagulation. Gastrointest Endosc 1988; 34:134-7.
11. Watson M, Hally RJ, McCue PA, Varga J,
Jimenez SA. Gastric antral vascular ectasia (watermelon stomach) in patients
with systemic sclerosis. Arthritis Rheum 1996; 39:341-6.
12. Kruger R, Ryan ME, Dickson KB, Nunez JF.
Diffuse vascular ectasia of the gastric antrum. Am J Gastroenterol 1987;
82:421-6.
13. Moss SF, Ghosh P, Thomas DM, Jackson JE,
Calam J. Gastric antral vascular ectasia: maintenance treatment with
estrogen-progesterone. Gut 1992; 33:715-7.
14. Rawlinson WD, Barr GD, Lin BP. Antral
vascular ectasia – the "watermelon" stomach. Med J Aust
1986;144:709-11.
15. Barbara G, De GR, Salvioli B,
Stanghellini V, Corinaldesi R. Unsuccessful octreotide treatment of the
watermelon stomach. J Clin Gastroenterol 1998; 26:345-6