Introduction
Parotid sparing is usually accomplished by irradiating the ipsilateral side of the neck while avoiding the opposite parotid. Tumor site, size, pathology and risk of lymphatic metastases dictate the specific anatomy and the amount of tissue that must be irradiated. It has been shown that approximately two third of the patients receiving radical radiation therapy for head and neck cancer experience weight loss1.
The amount of weight loss is maximal at three months after irradiation and recovers slowely thereafter. Weight loss during and immediately after treatment is due to acute mucosal reaction, whereas at three to six months later it is due to xerostomia and its sequelae. The greatest weight loss is experienced by patients whose parotid glands are irradiated during the course of treatment for cancers of the oral cavity and oropharynx. Parotid gland function can be spared with three dimensional treatment planning with unilateral head and neck cancers2.
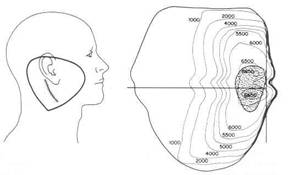
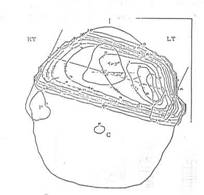
Retrospective analysis of 114 irradiated head and neck cancer patients showed that weight correlated with parotid function3,4. When both parotids were irradiated body weight fell to a nadir of minus 14 %, then gradually rose over the ensuing four years but never fully recovered. When one parotid was irradiated and the opposite was avoided, weight fell to a nadir of minus 4 % of the initial weight, fully recovered with in one year and paralleled the weigh of the controls whose parotids were not irradiated (Figure 1).
![]()
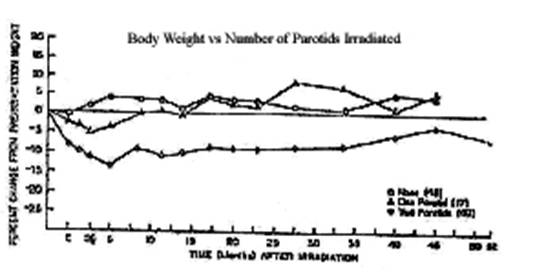
It was concluded that body weight depends on parotid function and can be maintained at normal levels as long as one parotid remains intact.
Rationale
There are certain cancers of the head and neck where small size, lateralization and diminished risk of contralateral metastases make it possible to localize the irradiation in such a way that the opposite parotid is spared. Consider the incidence of contralateral lymphatic metastases at presentation for lateralized cancers of the oral tongue, retromolar trigone, anterior tonsillar pillar, floor of mouth and tonsillar fossa as shown in Table 1, and for laryngo-pharynx Table 2.
Table-1: (Ref-12)- Incidence of contralateral lymphatic metastases at presentation as a function of site
|
Site |
No of patients |
% |
|
Nasopharynx |
82/169 |
48.5 |
|
Base of Tongue |
53/85 |
28.6 |
|
Pharyngeal wall |
25/149 |
16.7 |
|
Soft Palate |
13/80 |
16.2 |
|
Supraglottic Larynx |
43/267 |
16.1 |
|
Tonsillar Fossa |
16/140 |
11.4 |
|
Hypopharynx |
28/267 |
10.4 |
|
Oral Tongue |
16/302 |
5.3 |
|
Retromolar Trigone Area |
11/227 |
4.8 |
|
Floor of Mouth |
11/258 |
4.3 |
 Table-2:
(Ref 13)- Incidence of contralateral
lymphatic metastases as a function of origin for cancers of the larynx and
pharynx.
Table-2:
(Ref 13)- Incidence of contralateral
lymphatic metastases as a function of origin for cancers of the larynx and
pharynx.
|
Origin |
Min. F/Up |
Contralateral L.N/Total |
% |
|
Glassoepiglotis |
24 months |
17/35 |
49 |
|
Marginal Supraglottis |
24 months |
4/31 |
13 |
|
Central Supraglottis |
48 months |
3/29 |
10 |
|
Pyriform Sinus |
30 months |
4/49 |
8 |
|
Transglottic fixed |
24 months |
2/34 |
6 |
|
Transglottic mobile |
24 months |
0/11 |
0 |
Cancers of the valleculae, base of tongue and epiglottis are midline and obviously have an increased incidence of bilateral lymph nodes while those originating in the pyriform sinus, marginal and central supraglottis have a low incidence of spread to the opposite side of the neck5,6 Table 2.
Thus there are certain cancers of the head and
neck whose incidence of contralateral neck metastases is low enough that
parotid sparing is appropriate.
Dr. O’ Sullivan at Princess Margaret Hospital studied 86 tonsil and 26 oral cavity cancer patients with (T1-4, N0-N1) cancers treated with homo-lateral parotid sparing radiation techniques6. He found out that failures in the un-irradiated contralateral neck were unusual after minimum follow-up of 5 years Table 3.
Table 3 (Ref 13)- Lymphatic metastases to the un-irradiated contralateral side of the neck.
|
I/L Neck |
C/L neck Failure /Total |
% |
|
N0 |
1/18 |
1 |
|
N+ |
2/34 |
6 |
Sparing of the parotid glands translates into objective and subjective improvement of both xerostomia and quality of life in patients with head and neck cancers receiving radiation therapy7,8 .
This suggests that patients with appropriately selected lateralized lesions of
the oral cavity and tonsil can be irradiated with homo-lateral parotid sparing
techniques with out compromising over all control of the tumor.
TECHNIQUES
The techniques of irradiation used to spare anatomy and function are basically three:-
I. Limitation of Field Size for very small cancers with diminished risk of lymphatic spread, e.g., cancers of the true vocal cord.
II. Unilateral Wedge Pair or Electron Beam Techniques for small lateralized cancers with diminished risk of contralateral neck metastases, e.g., small cancers of the anterior tonsillar pillar.
III. The Use of Oblique Beams and three dimensional conformal treatment planning to cover the primary tumor and first echelon of lymphatics with sparing of the opposite parotid, e.g., cancers of the postero-lateral margin of the oral tongue.
1. LIMITED FIELD SIZE
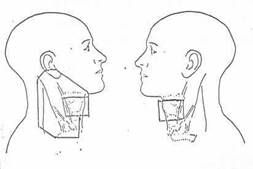
One of the ways of saving salivary functions is to avoid major salivary glands by using small fields. For example, small opposed fields are used to irradiate patients with cancers of the true vocal cord, supra-glottic larynx, hard palate and anterior oral tongue and floor of mouth. A single parotid can be saved by using parallel opposed photon fields limited to the larynx and electron beam for the ipsilateral neck when treating small lateralized cancers of the trans-glottic or supra-glottic larynx (Figure 2).

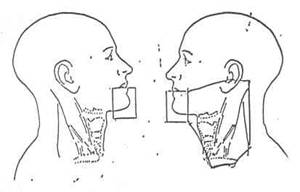
Similarly, parallel opposed photon fields in front-of the parotids along with electron beam irradiation of the ipsilateral neck can be used to save the opposite parotid of patients with small cancers in the anterior part of the oral cavity (Figure 3).
II. UNILATERAL TECHNIQUES
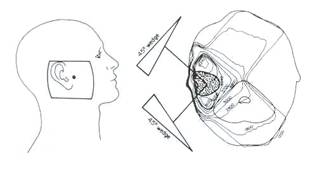
Wedge pair or electron beam techniques of irradiation can be used to irradiate patients with cancers of the skin, parotid, external ear (Figure 4,5)9 and buccal mucosa, tonsil and anterior tonsillar pillar. It is important to select patients with small lesions or surface lesions whose risk of contralateral neck metastases is small. Altogether small lateralized cancers of the oral cavity and faucial arch seldom exhibit lymphatic spread to opposite side of the neck. Thus unilateral parotid sparing techniques are rational and do much to preserve salivary function.
III. OBLIQUE BEAMS AND 3-DIMENSIONAL TREATMENT PLANNING
Oblique beams may be used to irradiate more posteriorly located cancer of the oral cavity not amenable to the small field of irradiation anterior to the parotid glands. The oblique beams include the ipsilateral parotid and the entire oral tongue but exclude the opposite parotid (Figure 6).
SUMMARY
Several authors have shown that xerostomia restricts nutritional intake and limits the ability of patients to maintain normal weight1,3. When both parotids are irradiated, patients never fully regain their normal weight, however if one parotid is irradiated the patients are able to fully recover their weight with in the year. There are certain sites in the head and neck where small and lateralized cancers with diminished risk of contralateral neck metastases can be treated with parotid sparing techniques, i.e., oral cavity, retromolar trigone, anterior tonsillar pillar, tonsillar fossa, and true vocal cord. In these sites it is appropriate to spare the opposite parotid and closely observe the un-irradiated neck.
Based on Dr. O’ Sullivans long term follow up of patients with cancers of the oral cavity and tonsil, we are encouraged that patients can be irradiated with homo-lateral parotid techniques with out jeopardizing loco-regional control6 . Hazuka et al and Maesa et al suggested that three dimensional treatment planning may allow the use of parotid sparing techniques in patients who otherwise would not have been considered candidates using conventional radiotherapy techniques10,11 .
References
1. Jhonston, Catherine A,. and Keane, Thomas J., Weight Loss in Patients Receiving Radical Radiation Therapy for Head and Neck Cancer: A Prospective Study, Journal of Parenteral and Enteral Nutrition, Vol. 6, No. 5, September/October 1982.
2. Jones RE, Takeuchi T, Eisbruch A, D’Hondt E, Hazuka M, Ship JA. Ipsilateral parotid sparing study in head and neck cancer patients who receive radiation therapy: results after 1 year. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996 Jun;81(6) : 642-8.
3. Marks, J.E., and Rao, D.V., Body Weight in Relation to parotid Irradiation, Unpublished Data.
4.
 Reddy
SP, Leman CR, Marks JE, Emami B. Parotid Sparing Irradiation for Cancer of the
Oral Cavity: Maintenance of Oral Nutrition and Body Weight by Preserving
Parotid Function. Am J Clin Oncol 2001 Aug;24(4):341-6.
Reddy
SP, Leman CR, Marks JE, Emami B. Parotid Sparing Irradiation for Cancer of the
Oral Cavity: Maintenance of Oral Nutrition and Body Weight by Preserving
Parotid Function. Am J Clin Oncol 2001 Aug;24(4):341-6.
5. Marks, J.E., Unpublished Data, 1989.
6. O’Sullivan, Brian, Lymphatic Metastases to the Un-irradiated Contralateral Side of the Neck in Patients with Squamous Cell Carcinoma of the Oral Cavity and Tonsil, Unpublished Data.
7. Chao KS, Deasy JO, Markman J, Perez CA, Purdy JA, Low DA. A prospective study of salivary function sparing in patients with head-and-neck cancers receiving intensity –modulated or three dimensional radiation therapy: Int J Radiat Oncol Biol Phys 2001 Mar 15;49(4): 907-16.
8. Hanson BS, Inglehart MR, Eisbruch A, Ship JA. Preserved salivary output and xerostomia-related quality of life in head and neck cancer patients receiving parotid-sparing radiotherapy. Oral Oncol 2001 Jan; 37(1):84-93.
9. Joseph R. Simposn and C.C. Wang: Principles and Practice of Radiation Oncology, 2nd ed, Fig. 30.8,30.10 and Fig.31.10. pp 662-3,683. Philadelphia, J.B. 1992.
10. Hazuka MB, Martel MK, Marsh L, Lichter AS, Wolf GT. Preservation of parotid function after external beam irradiation in head and neck cancer patients: a feasibility study using 3-dimensional treatment planing. Int J Radiat Oncol Biol Phys 1993 Oct. 20;27(3): 731-7.
11. Maes A, Weltens C, Flamen P, Lambin P, Bogaerts R, Liu X et al. Preservation of parotid function with uncomplicated conformal radiotherapy. Radiother Oncol 2002 May;63 (2): 203-11.
12. Carlos A. Perez. Tonsillar Fossa and Faucial Arch, Chapter 32, Eds. Carlos A. Perez and Luther W. Brady. Principles and Practice of Radiation Oncology 2nd ed. Fig. 32.4. pp. 693. and Fig. 33.2. pp. 715. Philadelphia J.B. Lippincott Raven, 1992.
13. Hameed S. and Marks JE. Parotid Sparing Radiation Techniques for Head and Neck Cancers. Syllabus for Head and Neck Rehabilitation International Conference and Work Shop. Dearborn, MI. March 14-18,1990