INTRODUCTION
Locally advanced (Stage III) carcinoma of the esophagus caries a
poor prognosis. Most of these patients have been treated with palliative
intention. In a study Roohulla et
al1 stated that 87 % of the patients presenting were of squamous cell histology and most of them were found in
stage III and beyond. These patients were mainly treated with palliative
radiation therapy, some of these were also treated with chemotherapy along with
radiation, but the overall survival remained poor. A few patients had also
palliative surgery prior to radiotherapy. In another study by Malik et,al2, only 54 % of patients with squamous
cell or adenocarcinoma of the esophagus could be
offered any surgical procedure, in 31 % patients palliative resection with
esophageal bypass was performed and in 13 % only bypass was possible .
Preoperative chemoradiation has been used in several series in an
attempt to downstage the disease, including that from
In another
series from Johns Hopkins School of medicine, Baltimore, USA.4 Of 39
patients who proceeded to surgery, 29 had responded to preoperative treatment,
11 achieved pathological complete response and 18 achieved a lower post
treatment stage, the two-year survival rate was 62 %. The two-year survival
rate for pathological complete responders was 91 % compared with 51 % in
patients with complete tumor resection with residual tumor. In a report from
Japan5,6, concurrent chemo-radiation
therapy followed by surgery was an effective, safe multimodality therapy for
patients with primary inoperable T4 squamous cell
carcinoma of the esophagus .
Does
pre-operative chemo-radiotherapy downstage the un-resectable
(Stage III/IV) esophageal cancers in our patients? To assess the efficacy of
neo-adjuvant chemo-radiotherapy followed by surgery, this regimen was followed
in Shaukat Khanum Memorial
Hospital (SKMCH).
MATERIALS AND METHODS
This observational study was conducted at the
department of radiation oncology SKMCH,
Primary objective was to compare
the efficacy of both regimens in down-staging the tumor. The secondary
objectives were to compare the pathological complete response rates in resected specimens in both regimens.
Patients of any age with ECOG
performance status of
0-2 and radiologically stage
III/IV locally advanced squamous cell carcinoma or adenocarcinoma
of lower thoracic esophagus who had completed neo-adjuvant chemoradiation
therapy. Patients with ECOG 3-4., uncertain diagnosis and with concurrent
malignancy other than skin cancer were excluded.
All patients
received external beam radiation-therapy 40 Gy in
twenty fractions at the rate of 200 cGy daily, five
days a week to antero-posterior and postero-anterior fields on Co-60 teletherapy
machine with five centimeter margin to tumor and also covering celiac axis
lymph-nodes (Fig.1). 10 Gy boost was delivered via oblique fields (Fig.2,3)
sparing the spinal cord to give total dose up-to 50 Gy.
Chemotherapy was given concomitantly with radiation using one of the following
regimens -
Arm A - 5FU 500 mg/m2 intravenous push (IVP) first 5 and last
5 days of radiation half to one hour before radiation.
Arm B - 5FU 1 Gm/ m2/Day 96
hour continuous infusion (CIV) and Cisplatin70 mg/ m2 eight hour
infusion on day one and twenty eight of radiation.
Four to six weeks after completion of chemoradiation C.T/MRI scan of the chest was repeated and
patients were offered surgery (Transhiatal esophagectomy), if the disease had become resectable and surgical specimen was submitted to
histopathology to see the response.
RESULTS
Characteristics and histopathology of 35 patients who
fulfilled the inclusion criteria are given in table 1 and 2 respectively in
each treatment arm. Twenty-six patients received arm A
regimen, in 13 the disease was made resectable and
surgical specimen in two of them showed pathological complete response. Of
thirteen patients who had un-resectable disease, 3
lost to follow-up (These were considered to have progressive disease), eight
had progressive disease to celiac lymph nodes and bone metastases, and in two surgery was not carried out because of the development of
myocardial infarction.
Table-1: Patient characteristics
|
Variables |
Arm A (# 26) |
ARm b (#9) |
|
Age ≤
50 year >
50 year |
12
(46%) 14
(54%) |
07
(77%) 02
(22%) |
|
Sex Male Female |
17
(65%) 09
(35%) |
03
(33%) 06
(67%) |
On the other hand out of nine patients
who received arm B regimen, in seven the disease was made resectable
and surgical specimen in five patients had no viable tumor. In two with unresectable disease, one had progressive disease (Ascites) and one lost to follow-up. These results are
summarized in table 3.
Table 2- Histopathology of patients
|
Histopathology Poorly
differentiated squamous cell carcin-oma Moderately
differentiated squamous cell carcin-oma Adenocarcinoma |
Arm A (n=26) 06
(23%) 16
(61%) 04
(15%) |
Arm B (n=9) 04
(44%) 04
(44%) 01
(11%) |
Table 3- Resectability
rates.
variable
|
arm a (N=26) |
arm b (n= 09) |
|
Resectable |
13 (50%) |
07 (77%) |
|
Un-resectable |
13 (50%) |
02 (22%) |

Figure-1: Simulation film of AP/PA field to 40 Gy.
Lower border covers the celiac axis
DISCUSSION
Locally advanced esophageal
carcinoma (Stage III/IV) is un-resectable disease and
caries a poor prognosis.1 Curative surgery of thoracic esophageal
cancer involves a subtotal or total esophagectomy.
Surgery has been the standard treatment for thoracic esophageal carcinoma, but
two largest series by Erlam and Cunha-Melo7,
review 122 papers involving more than 83,000 patients treated primarily by
surgery. The overall 5-year survival rate for patients with resected
tumors was 12 %. Patients treated with palliative intention had a survival
range of 2-6 months. Studies by Walsh et al8
and Urba et al9 report 6 % and 15 % 3 year
survival in the surgery alone arm, respectively.
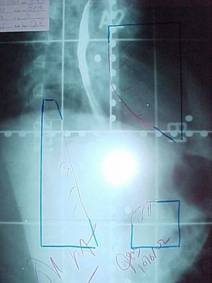
Figure-2: Simulation film of right
anterior oblique field sparing the spinal cord
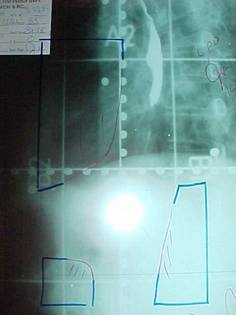
Figure-3: Simulation film of left anterior
oblique field sparing the spinal cord
Poor patient
outcome with surgery alone has led to the development of alternative primary
treatment or adjuvant therapy in conjunction with surgery. When the disease is
in-operable because of tumor extent or medical contraindications, radiation
alone has been given. In a thorough review Earlam and
Cunha-Melo10 analyzed 49 series involving more than 84,000 patients
treated primarily with radiation between 1954 and 1979. They found overall
survival rates at 1,2 and 5 years to be 18 %, 8 % and
6 % respectively.
Data from the
In our patients
at SKMCH, all the un-resectable patients were offered
preoperative chemo-radiotherapy using two different chemotherapy regimens. One
arm A, as out patient basis. The arm B consisted of continuous infusion. From
the results it can be seen that patients receiving continuous infusion of two
drugs had better resectability rates and moreover the
pathological complete response was superior in the later regimen. At present,
four phase II trials have reported on a pre-operative combination of Cisplatin, Paclitaxel, and
radiotherapy.12-14
REFERENCES
1.
Roohulla K, Burdy G,M,
Hamdani S,R, Javaid I, Kamran S, Nusrat J. Cancer of esophagus,
Ten year experience at CENAR,
2.
Malik AM, Khan AH, Khan B, Bashir
H. Surgical bypass for palliation of Carcinoma Esophagus. Pak Armed Forces Med
J 1999;49(
3.
Slater MS,
4.
Heath EI, Burstness BA, Heitmillar RF,
Salem R, Kleinberg L, Kinsely P, et al. Phase II
evaluation of pre-operative chemoradiation and
postoperative adjuvant chemotherapy for squamous cell
and adenocarcinoma of the esophagus: J clin oncol 2000; 18(4): 868-76.
5.
Yano M, Tsujinaka T, Shiosaki H, Inoue M,
Doki Y, Yamamoto M, et al. Concurrent chemotherapy (5
FU and Cisplatin) and radiation therapy followed by
surgery for T4 squamous cell carcinoma of the
esophagus. J Surg Oncol
1999; 70(1):25-32.
6.
Chan An, Wong A. Is combined chemothrapy
and radiation therapy equally effective as surgical resection in localized
esophageal carcinoma? Int J. Radiat
Oncol Bio Phys 1999; 45(2): 265-70.
7.
Earlam R, Cunha-Melo JR. Oesophageal squamous cell
carcinoma:
8.
Walsh TN, Noonan N,
Hollywood D, Kelly A, Kelling N, Hennessy TPJ. A
comparison of multimodality therapy and surgery for esophageal adenocarcinoma. N Eng J Med 1996;335:462-7.
9.
Urba SG, Orringer MB, Turrisi A. Randomized trial of preoperative chemoradiation versus surgery alone in patients with locoregional esophageal carcinoma. J Clin
Oncol 2001;19:305-9.
10. Erlam R, Cunham-Melo JR.
Esophageal squamous cell carcinoma: II. A critical
review of radiotherapy. Br J Surg 1980;67:457-62.
11. Forastiere AA, Orringer MB, Perez-Tamayo C. Preoperative chemoradiation
followed by transhiatal esophagectomy
for carcinoma of the esophagus: final report. J Clin Oncol 1993:11:1118-23.
12. Adelstein DJ, Rice TW,
13. Blanke C,Chiappori
A, Epstein B. A phase II trial of neo-adjuvant paclitaxel
and cisplatin with radiotherapy followed by surgery
and postoperative taxol with 5FU and leucovorin in patients with locally advanced esophageal
cancer. Proc Am Soc Clin Oncol
2000;19:248a.
14. Urba SG, Orringer M, Iannettoni M. A phase II trial of preoperative cisplatin, paclitaxel, and
radiation therapy before transhiatal esophagectomy (THE) in patients with locoregional
esophageal cancer (CA). Proc Am Soc Clin Oncol 2000;19:248a